Historically, clinical emphasis has been placed on toxin removal in dialysis using numerous technological advances, complex methods of analyzing clearance and improved dialyzer membranes. However, fluid management in hemodialysis has remained largely unchanged. With Crit-Line® technology, providers can now access information that can help improve fluid management in hemodialysis patients. Please note that Crit-Line technology does not provide a treatment algorithm and does not directly intervene in the dialysis treatment.
Managing fluid during hemodialysis has always been a challenge. Based on the data that the Crit-Line technology provides, the dialysis technician may intervene (i.e., increase or decrease the rate at which fluid is removed from the body) in order to potentially remove the maximum amount of fluid from the dialysis patient without the patient experiencing the common symptoms of dialysis which include nausea, cramping and vomiting. Therefore, it has been suggested that better fluid management can help improve dialysis patient care.1
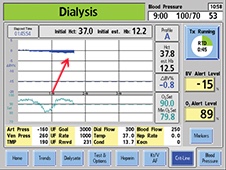
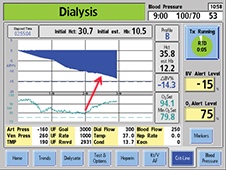
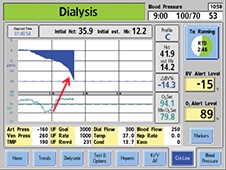
Crit-Line technology provides objective data and visually displays the relative blood volume slope, which indicates the balance between the dialysis patient's vascular refill and ultrafiltration rates. Based on that information, the provider can intervene and adjust the rate of fluid removal in order to remove the maximum amount of fluid. The slopes or profiles that are displayed by Crit-Line technology are typically categorized as A, B or C and are defined as follows:
Caution: Federal (US) law restricts these devices to sale by or on the order of a physician.
Note: Read the Instructions for Use for safe and proper use of these devices. For a complete description of hazards, contraindications, side effects and precautions, see full package labeling.
© 2017-2021 Fresenius Medical Care. All Rights Reserved. Fresenius Medical Care, the triangle logo, 2008T BlueStar, Crit-Line and CLiC are trademarks of Fresenius Medical Care Holdings, Inc. or its affiliated companies. All other trademarks are the property of their respective owners. P/N 102249-01 Rev I 04/2021