
A Perspective on the Next Generation of Value Based Care in Kidney Disease
How can value based care (VBC) better serve patients with kidney disease? Fresenius Medical Care North America (FMCNA) is leveraging its expertise to help design programs that balance the needs of patients, providers, and payors. Next-generation programs will most likely encompass a greater range of the disease, from chronic kidney disease (CKD) through end stage renal disease (ESRD) and kidney transplant. This longitudinal model can offer patients less fragmented and episodic care, a broader choice of treatments, and improved outcomes over the course of many years.
FMCNA became a pioneer in population health management in 2006 by extending a VBC contract to ESRD patients in an early Centers for Medicare and Medicaid Services (CMS) demonstration. FMCNA continues to lead in this space and is preparing for the next generation of VBC.
VBC programs continue to mature across the US healthcare landscape, driven by the insurance providers (payors) and the Center for Medicare and Medicaid Innovation (CMMI). One of the most successful of these programs, the Comprehensive ESRD Care (CEC) Model, commonly referred to as the ESRD Seamless Care Organization (ESCO) demonstration, is in its fourth year of a five-year program, with FMCNA operating nearly two-thirds of all ESCOs and caring for 80 percent of the beneficiaries. Because the ESCOs create financial savings and improve care, CMMI is developing the next generation VBC program modeled on the successful ESCO program to continue beyond 2020.
CMMI has indicated that the next generation renal program will likely encompass a greater range of the disease, from CKD through ESRD and kidney transplant. The US government's July 2019 announcement of the Advancing American Kidney Health initiative proposes to increase transplantation, home dialysis, and value based models including the introduction of voluntary and mandatory payment models beginning in January 2020. ESRD Treatment Choices (ETC) is a required model that adds new financial incentives to encourage dialysis at home and intends to enroll half of the nation's Medicare ESRD beneficiaries by randomly aligning beneficiaries using a specified geographic framework. To avoid penalizing ESRD providers with sicker patients, the model would risk adjust the home dialysis and transplant rates used for purposes of the performance payment adjustments. The administration is rolling out additional optional payment models through the CMMI.
EXPANDING THE NUMBER OF PATIENTS IN VBC CONTRACTS
Most renal patients never progress to dialysis, yet CKD is often overlooked in many VBC programs. Based on the US government's kidney-focused policy announcement, the successes of the ESCO program and public comment from CMMI and Health and Human Services (HHS) officials, FMCNA anticipates that most future renal VBC programs will encompass CKD care, in-center dialysis, home dialysis, transplant, and post-transplant care, removing many of the artificial boundaries that kidney disease and treatment modalities traditionally have been segmented into and managed independently. Beyond improvements in more holistic patient care, a more expansive VBC program solves one of the age-old dilemmas of health insurance: beneficiary turnover. It can be challenging for payors to invest in long-term outcomes when beneficiaries may leave the plan before such investments yield financial results. A broader kidney program covering a larger spectrum of the disease state creates a consistency with patients and gives organizations like FMCNA increased financial incentive to invest in patient care and improved health outcomes by providing population health management over the course of years. After all, kidney disease is a longitudinal chronic illness, with dialysis only one part of the care continuum.
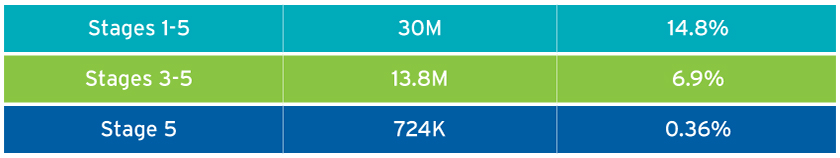
Based on the National Health and Nutrition Examination Survey (NHANES) conducted by the United States Renal Data System (USRDS), 14.8 percent of patients surveyed have stages 1-5 and 6.9 percent have stages 3-5.1 There were 124,675 new dialysis patients in 2016.2 Less than half of 1 percent of adults are receiving dialysis, and fewer than 1 in 30 patients with CKD receive dialysis (Figure 1). Because there are many more patients with CKD than ESRD at any given point in time, an expanded VBC model that includes CKD would provide FMCNA the opportunity to improve outcomes for a greater number of people than just those with ESRD.
FIGURE 1 | Prevalence of chronic kidney disease
Delaying renal disease progression can save the payor—and, in some cases, the taxpayer via Medicare contributions—as much as $48,000 per year per patient.3
MORE INTEGRATED CARE ACROSS THE RENAL DISEASE CONTINUUM
It is well established that starting dialysis is very difficult for patients socially, emotionally, and financially. Planning and preparation can not only help patients address and mitigate these challenges but also improve outcomes during this transition. FMCNA's Renal Care Coordinator (RCC) program engages patients by providing care coordination prior to the initiation of dialysis and during a patient's first 120 days receiving dialysis. In 2017, this intensive care coordination resulted in:4
- A 23 percent reduction in hospital admissions
- 9 percent more patients selecting home dialysis modalities
- Fewer dialysis treatments missed
- A 10 percent reduction in spending on total health care compared to non-RCC patients
Specific benefits of VBC programs that include the full renal disease spectrum are:
- Development of longitudinal care plans.
According to Cerner, a health information technology company, longitudinal care planning is not provided to patients because of a lack of incentives to the health care organizations.5 A single model for care coordination may eliminate fragmentation and episodic care. One example of an opportunity for improvement is diabetes care. According to USRDS, 36 percent of CKD patients have diabetes. Using longitudinal health plans and additional care coordination to manage common comorbidities should improve outcomes.
- Management of CKD progression.
- Slowing or delaying the progression of CKD and reducing the frequency that patients crash (start urgently without ideal preparation) into dialysis are the goals or are desirable.6 Under a VBC care program, earlier intervention may result in disease progression delays thanks to:
- A centralized monitoring and tracking program
- Referrals for improved nutrition and diet management
- Improved medication management and monitoring to help avoid nephrotoxic drugs
- An expanded care team's coordinated focus on mitigating conditions that worsen renal disease, such as diabetes and hypertension
- Preemptive transplantation
- Such care coordination would focus closely on efforts to control blood pressure, reduce proteinuria with angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers, and reduce some cardiovascular risks by providing enhanced support to stop tobacco use.
- Slowing or delaying the progression of CKD and reducing the frequency that patients crash (start urgently without ideal preparation) into dialysis are the goals or are desirable.6 Under a VBC care program, earlier intervention may result in disease progression delays thanks to:
- Vascular care coordination.
There is more opportunity to align and coordinate with vascular access care. The RCC program resulted in a 15 percent reduction in patients who started dialysis with a catheter.7 Permanent access is correlated with reduced admissions, less chance for infection from a temporary catheter, and a reduction in the total cost of care.
- More patient choice.
More emphasis on transplant, conservative care (no dialysis), and modality selection should result in increased treatment options with proven better outcomes for patients, including peritoneal dialysis and home hemodialysis. Enhanced education and earlier and more frequent discussions create the opportunity to choose a modality that best suits an individual's lifestyle and needs. Coordinating the competition and aggregation of the prerequisite transplant screening evaluations would result in more patients successfully completing this process and ultimately being listed as a candidate for transplant.
- Mitigation of external influences.
Stressing conservative care or transplant in a CKD VBC program mitigates potential bias of treatment recommendations. A study of CKD patients over 80 years of age with severe comorbidities found there was no difference in physical or mental function, but the conservative group spent fewer days in the hospital with lower overall cost of care.8 Yet some patients are not offered the option of getting a transplant or foregoing dialysis due to the way the current delivery system rewards providers. The next generation of VBC should incorporate more options, including conservative care without starting dialysis in patients who would experience a negative quality of life impact, such as the frail and elderly. Additionally, better education about palliative care and hospice care, as well as closer alignment of the palliative care provider network with the Accountable Care Organization (ACO), will be commonplace.
- Post-transplant management.
Post-transplant care requires attention to detail and coordination among caregivers and the patient. In 2018, there were 21,166 transplants, with 94,892 patients listed as waiting for transplant.9 In the next generation of VBC programs, incentives are aligned to offer patients the necessary support to ensure that transplants are effective and lasting. As of Q1 2019, there are gaps in post-transplant care and confusion between roles of the transplant center, nephrologist, and primary care physicians. The National Kidney Foundation lists 17 areas of care that a transplant patient needs to consider—several are well beyond renal function and immunosuppression-related care.10 In a VBC care program, the care team is incentivized to ensure all aspects of the renal transplant patient's needs are addressed and that the transplant remains viable for as long as possible. The care and care coordination needs are complex.11 Additional post-transplant care would include better preparation for failing transplants, including establishing permanent vascular access for anticipated return to dialysis.
- Improved patient satisfaction.
This is possible with additional support provided to the patient in the VBC program. Activities could be driven using data and a population health approach to allow for better and more targeted care. FMCNA—with its value based care team (Fresenius Health Partners), aligned nephrologists, clinics, vascular access centers, vascular access care providers, transplant specialists, partnerships with transplant centers, and health systems—is perfectly aligned and well prepared to coordinate and manage the care of the renal patient.
EFFECTIVE FINANCIAL ALIGNMENT OF ACCOUNTABLE CARE ORGANIZATIONS
The next generation of VBC will have enhanced financial alignment. Payors seek to reduce the total cost of care and improve patient outcomes and lifestyles by having VBC programs designed to delay the progression to ESRD, facilitate more transplants, and encourage patients to seek home dialysis as their dialysis modality. The at-risk patient cohort must expand beyond ESRD to include pre- and post-ESRD to achieve these goals.
Stronger connections between payor (or CMS) and the participants (FMCNA and partners) with more financial transparency and increased flexibility will deliver innovative care by eliminating barriers to renal care inherent in a fee-for-service delivery system.
Some specifics of the next generation of VBC programs will hopefully include:
- A monthly capitated cost trend established in advance
- A robust risk adjustment program similar to the Medicare Advantage program
- Stable patient alignment into the program (movement in and out of a program can make it extremely difficult to effectively manage care over longer periods of time)
Further improvements to VBC programs will likely include payor- supported enhanced benefits and, within CMMI demonstrations, the use of waivers, deviating from the established limitation of fee-for-service in Medicare. These will include:
- Allowance for spending on patient engagement technology and monetary incentives
- Enhanced home visits and care
- Telehealth
- Abolishment of the three-day hospital admission rule before being admitted to a skilled nursing facility
- Open shared savings distributions to a wider group of participants
- Developing exceptions to the Anti-Kickback Statute and Stark Law for aspects of care that benefit from integration
- Allowance for spending on nonmedical care and services
Having a VBC model that includes CKD, dialysis, and post-transplant care allows for patient participation over a greater duration of their renal disease state. This results in improved care continuity, slower disease progression, better ESRD care choices, higher home dialysis modalities selection, more transplant options, better post-transplant care, and a reduction in the total cost of care. The next generation of renal value based programs will include more patients, participating for a longer period, and they will benefit from longitudinal care integration. FMCNA is poised to help design and deliver the next generation of programs to benefit patients, payors, and providers alike.
Meet Our Expert
ANDREW ARONSON, MD, FACEP
Senior Vice President, Chief Clinical Operations Officer, Fresenius Health Partners
Andy Aronson oversees the clinical aspects of ESRD Seamless Care Organizations and the commercial ESRD programs. He is a Board-Certified Emergency Physician, a fellow of the American College of Emergency Physicians, and on the editorial board of the Journal of Population Health Management. He completed medical school at Drexel University College of Medicine and emergency medicine residency at Brigham and Women's Hospital and Massachusetts General Hospital.
References
- United States Renal Data System (USRDS). "CKD in the general population," chap. 1, vol. 1, 2018 annual data report. https://www.usrds.org/2018/view/v1_01.aspx.
- USRDS. "Incidence, prevalence, patient characteristics, and treatment modalities," chap. 1, vol. 2, 2018 annual data report. https://www.usrds.org/2018/view/v2_01.aspx.
- Johnson DS, Kapoian T, Taylor R, Meyer KB. Going upstream: coordination to improve CKD care. Semin Dial 2016 Mar-Apr;29(2):125-34. doi: 10.1111/sdi.12461.
- (Internal Fresenius Health Partners data).
- Bisbee D. Using the HER to impact episodic and longitudinal care plans. Cerner blog, Nov. 6, 2017. https://www.cerner.com/blog/using-the-ehr-to-impact-care-plans.
- USRDS. CKD in the general population. https://www.usrds.org/2018/view/v1_01.aspx.
- (Internal Fresenius Health Partners data)
- Wouter R., Verberne JD, Kelder JC, et al. Value-based evaluation of dialysis versus conservative care in older patients with advanced chronic kidney disease: a cohort study. BMC Nephrology 2018;19:205.
- UNOS. Waiting list candidates by organ type. https://unos.org/data/transplant-trends/waiting-list-candidates-by-organ-type/; and US Department of Health and Human Services Organ Procurement and Transplantation Network data, https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/#.
- National Kidney Foundation. A to Z health guide: Care after kidney transplant. Accessed May 1, 2019. https://www.kidney.org/atoz/content/immunosuppression.
- Gupta G, Unruh ML, Nolin TD, Hasley PB. Primary care of the renal transplant patient. J Gen Intern Med 2010 Jul;25(7):731-40.


