
How to Help a Patient Succeed at Home Dialysis
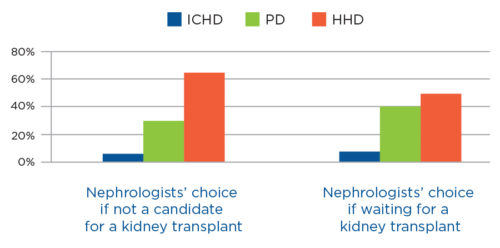
Over 85 percent of patients with end stage renal disease (ESRD) are eligible for different dialysis treatments, yet only 10 percent of them choose home dialysis over the conventional in-center hemodialysis (ICHD).1,2 Peritoneal dialysis (PD) or home hemodialysis (HHD) are viable options for patients with ESRD. Research identifying the relationship between different kidney disease treatments and patients' outcomes has been a subject of growing interest in the past decade. As of Q4 2016, research suggests that home dialysis treatments are as effective as in-center dialysis treatments and may result in better health outcomes and quality-of-life satisfaction for the patient.3 In fact, for most nephrologists, it is also the preferred modality in the event they were to develop ESRD themselves (Figure 1). Despite the potential benefits of home dialysis, studies suggest that this option is not properly introduced to patients, leading to misinformation and a perfectly viable modality being underused.4
CRITERIA FOR HOME DIALYSIS SUCCESS
Availability of information is indeed a major obstacle for patients.5 Patients view renal replacement therapy as a complex procedure, and they assume dialysis requires medical supervision in a clinical setting. As a result, patients are reluctant to consider home dialysis. Research suggests that in order for patients to both select and be successful with home dialysis, there are several important tools/guidelines that need to be considered:6-8

Each of these factors can be managed with strategies that may establish a permanent home dialysis treatment.
OFFERING TIMELY, TEAM-BASED EDUCATION
If home dialysis is not discussed with patients, they automatically assume it is not a viable option for them. Educating patients about all dialysis modalities, irrespective of whether they maybe suitable home dialysis candidates, ensures they are aware of all available options.9 Thereafter, the patient and clinician can decide the best option given the patient's health status, goals, and lifestyle.10
It is well-documented that patients undertaking comprehensive pre-dialysis education and adequate preparation tend to select home therapy and achieve better clinical outcomes regardless of their modality choice.11-14 Successfully delivering this education requires adequate timing and acceptance of disease progression. These studies suggest that it is best to instruct patients when an estimated glomerular filtration rate of less than 30 mL/min (stage IV chronic kidney disease) has been reached.15
This education is most beneficial when provided by a multidisciplinary team that includes a nephrologist, nurse, dietitian, and social worker.16 In most cases, however, a nephrologist will not have sufficient time to dedicate to one-on-one education sessions for the patient. It is advisable to engage nurse education specialists for the instruction process.
To make this education process successful, a few concepts are recommended:
- Conduct a combination of one-to-one and group educational sessions to enhance the impact of the delivered information.
- Emphasize to patients that they can safely perform dialysis at home—which is something nurses are well positioned to advocate for.
- Assure patients and caregivers that home dialysis is, in fact, the treatment of choice for many ESRD patients, a message that could also be effectively delivered by nurses.
PROVIDING TRAINING TO MAKE HOME DIALYSIS COMFORTABLE AND PERSONAL
Training is key to ensuring a patient builds a strong commitment to the home-based modality. Initial discussion should focus on the availability of adequate space, resources, and infrastructure.
Patients are likely to be more receptive to training that is tailored to their particular needs. This will enable every patient to complete the program with confidence in their ability to manage their home dialysis care. A “nurse navigator” can also assist the patient by guiding them through the steps.
There are no studies evaluating the optimum duration for home dialysis training, so it is recommended the training continue until the patient demonstrates competency and comfort with the procedures they will need to perform during home dialysis treatment. A successful training program—one that engages the patient with the training process and their own care—should include:17,18
- A combination of visual and auditory educational materials
- Delivery of a maximum of four key messages every hour of training
- Strategic periodic breaks every couple of hours
SUPPORTING FAMILY/CAREGIVER WITH PATIENT ASSISTANCE
Home dialysis patients typically rely on family and/or friends for support and caregiving duties. Caring for a chronically ill patient is a well-documented source of stress for the informal caregiver, impacting the caregiver's psychological, behavioral, and physical health.19 It is important to note that a caregiver's perspective can influence the patient's decision to choose home dialysis versus in-center dialysis. The care provider can be a positive influence on the patient, provide moral support, and strengthen compliance with dietary restrictions, treatment prescription, and medications at home. Consequently, the physical and psychological preparation of a caregiver is just as important as patient training for a successful home dialysis program.
A few home dialysis programs have successfully engaged nurses or patient-care technicians at home to lessen the burden on caregivers. Providing adequate home dialysis support services and scheduling planned breaks for caregivers are important ways to manage caregiver burden.
COMMUNICATING OFTEN TO INCREASE ADHERENCE TO TREATMENT
Flexible treatment schedules and an ability to dialyze in the comfort of a patient's home are two advantages of home dialysis; however, the demands of managing a home dialysis program may lead to non-adherence, adversely impacting clinical outcomes.
An estimated 10-20 percent of peritoneal dialysis (PD) patients intentionally fail to adhere to their dialysis prescription. In several studies, continuous ambulatory peritoneal dialysis (CAPD) patients were noted to have higher non-adherence levels than automated peritoneal dialysis (APD) patients.20-22 Furthermore, some HHD patients also report non-adherence to dialysis prescription. A potential cause of non-adherence may be poor coping strategies linked to the duration and frequency of HHD treatments.23
Adherence can be determined by reviewing dialysis logs and performing inventory checks. Avenues of monitoring home dialysis adherence may include installing advanced home dialysis machines; monitoring patient treatments by connected health applications; frequent patient reminders via e-mail, text messaging, or phone calls; and improved patient education.24
MAKING SPACE FOR HOME DIALYSIS
Because home dialysis patients can receive 50 to 60 boxes of supplies every month, patients should be told that they will need to have adequate storage space and plan for monthly inventory management. In addition, they will need to determine where in their home they prefer to dialyze themselves. Effectively managing inventory will prevent the patient from running out of supplies and risking poor treatment adherence. Technology-based tools are readily available to assist patients with inventory management.
PLANNING A SCHEDULE
In order for home dialysis to be successful, the patient has to manage time effectively. A nurse education specialist can help by taking the patient's daily routine into consideration and assist with integrating dialysis treatment into their daily life. Time management is less of an issue with nocturnal dialysis; however, a patient who chooses to dialyze during the day may benefit from designing a weekly treatment schedule. The effort put forth to develop time management skills may result in patients better adhering to home dialysis.
SUMMARY
Home dialysis modalities, including peritoneal dialysis and hemodialysis, are options suitable for the majority of dialysis patients and are perfectly acceptable alternatives to in-center dialysis. Home dialysis is effective and offers a more personalized, patient-centered alternative. Patients are not normally aware that this option is available to them. Increasing awareness, providing patients and caregivers with timely information, and guiding them before and during the process may encourage more patients to select home modality—and be more likely to succeed at it.
Meet Our Expert
DINESH CHATOTH, MD
Associate Chief Medical Officer, Fresenius Kidney Care
Dr. Chatoth is currently supporting the evolution of Home Therapies at Fresenius Kidney Care. He is Medical Director for a Fresenius Kidney Care hemodialysis unit in Lawrenceville, Georgia, and former Chairman of FMCNA's East Medical Advisory Board. A member of the FMCNA Corporate Medical Advisory Board and the Fresenius Physician Technology Group, Dr. Chatoth is President and CEO of Georgia Nephrology in Atlanta and lectures extensively on chronic kidney disease management.
References
- Merighi JR, Schatell DR, Bragg-Gresham JL, et al. Insights into nephrologist training, clinical practice, and dialysis choice. Hemodial Int. 2012;16(2):242-251.
- Mendelssohn DC, Mujais SK, Soroka SD, et al. A prospective evaluation of renal replacement therapy modality eligibility. Nephrol Dial Transplant. 2009 Feb;24(2):555-61.
- Rivara MB, Mehrotra R. The changing landscape of home dialysis in the United States. Curr Opin Nephrol Hypertens. 2014;23(6):586–591.
- Wuerth DB, Finkelstein SH, Schwetz O, Carey H, Kliger AS, Finkelstein FO. Patients’ description of specific factors leading to modality selection of chronic peritoneal dialysis or hemodialysis. Perit Dial Int. 2002. Mar-Apr;22(2):184-90.
- Marron B, Martinez Ocana JC, Salgueira M, et al. Analysis of patient flow into dialysis: Role of education in choice of dialysis modality. Perit Dial Int. 2005;25(Suppl 3):S56–S59.
- Ibid.
- McLaughlin K, Jones H, VanderStraeten C, et al. Why do patients choose self-care dialysis? Nephrol Dial Transplant. 2008;23:3972–3976.
- Mehrotra R, Marsh D, Vonesh E et al. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int. 2005;68(1):378-390.
- McLaughlin et al. Why do patients choose self-care dialysis?
- Hutchinson and Courthold. Enabling self-management.
- McLaughlin et al. Why do patients choose self-care dialysis?
- Marron et al. Analysis of patient flow into dialysis.
- Mehrotra et al. Patient education and access of ESRD patients.
- Hutchinson AJ, Courthold JJ. Enabling self-management: selecting patients for home dialysis? Nephrol Dial Transplant. 2011;4(suppl 3):iii7-iii10.
- Goldstein M, Yassa T, Dacouris N, McFarlane P. Multidisciplinary predialysis care and morbidity and mortality of patients on dialysis. Am J Kidney Dis. 2004;44(4):706–714.
- Hutchinson and Courthold. Enabling self-management.
- Manns BJ, Taub K, Vanderstraeten C, et al. The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: a randomized trial. Kidney Int. 2005;68:1777–1783.
- Bernardini J, Price V, Figueiredo A. On behalf of the International Society for Peritoneal Dialysis Nursing Steering Committee. Peritoneal dialysis patient training. Perit Dial Int. 2006;26:625-632.
- Bevans MF, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA. 2012 Jan 25;307(4):398–403.
- Carey HB, Finkelstein SH, Santacroce et al. The impact of psychosocial factors and age on CAPD dropout. Adv Perit Dial. 1990;6:26-29.
- Blake PG, Korbet SM, Blake R, Bargman JM, Burkart JM, et al. A multicenter study of noncompliance with continuous ambulatory peritoneal dialysis exchanges in US and Canadian patients. Am J Kidney Dis. 2000;35:506-514.
- Bernardini J, Nagy M, Piraino B. Pattern of noncompliance with dialysis exchanges in peritoneal dialysis patients. Am J Kidney Dis. 2000;35:1104-1110.
- Nearhos J, Van Eps C, Connor J. Psychological factors associated with successful outcomes in home haemodialysis. Nephrology (Carlton). 2013;18:505-509.
- Russell CL, Cronk NJ, Herron M, et al. Motivational Interviewing in Dialysis Adherence Study (MIDAS). Nephrol Nurs J. 2011;38(3):229-236.


