
Improving Access to Kidney Transplantation for Dialysis Patients with ESRD
Kidney transplantation is the treatment of choice for the majority of patients with End Stage Renal Disease (ESRD). There are significant benefits in quality of life and patient survival, particularly for patients who receive a preemptive transplant and also for patients who receive a transplant from a living donor. Fresenius Medical Care North America (FMCNA) is committed to expanding patient access to transplantation.
Fresenius Kidney Care, the dialysis services division of FMCNA, is committed to removing barriers between our clinics and transplant centers. This collaboration is a natural extension of the value based model focused on improving population-based
Several issues are important in the effort to facilitate patient access to kidney transplant opportunities:
- Increased regulatory attention to improving referral kidney transplant rates.
- Recent revisions to the kidney allocation system (KAS) and implications for transplant center behavior
- Opportunities for collaboration between dialysis facilities and transplant centers, which would also improve the quality of care delivered in dialysis units
INCREASING REGULATORY ATTENTION
Increasing patient access to kidney transplantation is a top priority for CMS and therefore the ESRD Networks. Providing and documenting evidence of patient transplant education are required in the ESRD conditions for coverage (CfCs).1 In addition, CfCs require that all patients are evaluated to determine if they are candidates for transplantation.
In 2013 ESRD Network 6 (covering North Carolina, South Carolina, and Georgia) identified a pattern of very low transplant referral rates, with a specific concern for African American patients. To address these concerns, the Reducing Disparities in Access to Kidney Transplantation (RaDIANT) Community Study was initiated by the Southeastern Kidney Transplant Coalition and ESRD Network 6, involving medical directors, regional managers, unit nurses, and staff. The network implemented a multifaceted program to improve the overall transplant referral rates and reduce disparities in access to transplants for minority patients (Figure 1).2
The results of this program demonstrated an overall increase in referral rates to 17.4 percent for patients who participated in the RaDIANT intervention versus 10.2 percent for patients who received standard transplant education. The study also demonstrated an increase in the rate of referrals among African American patients (Figure 2).3,4
REVISIONS TO THE KIDNEY ALLOCATION SYSTEM
The Kidney Allocation System (KAS), a system designed to allocate kidneys to those on the kidney transplant list, was revised in January 2015.5 Here are some specific features of this complex and dynamic system:
- Candidate waiting time is designated by a point system: One year of wait time on the transplant list equals 1.0 point in terms of priority for a transplant.
- Preemptive candidate listing continues to be permitted for candidates with eGFR of less than 20 cc/min.
- For candidates with ESRD, waiting time is backdated to the start date of ESRD (as listed on the CMS 2728 form).
- Highly sensitized patients with a cPRA of greater than 98 percent are listed with a higher priority.
- Donated kidneys are assessed with a Kidney Donor Profile Index (KDPI) score.
- Transplant candidates are assessed with an Estimated Post-Transplant Survival (EPTS) score (low KDPI scores are preferentially assigned to candidates with low EPTS scores)
Simply increasing the rate of candidate referrals for evaluation does not guarantee an increase in the number of patients actually receiving transplants. The new allocation system poses challenges for dialysis clinics due to the emphasis on a benchmark for the rate of transplant referral rather than the rate of a successful transplant.
For example, many unsensitized patients new to ESRD without a potential living donor may not benefit from evaluation and listing until they have accumulated several years of waiting time (“points”), and some efficiency-minded transplant centers may decline to evaluate patients until they accumulate sufficient ESRD time to reduce the need for repeated screening tests. In such circumstances, valiant efforts to increase rates of transplant referrals may not always result in higher listing rates, much less higher rates of transplantation. To successfully increase the transplant rate, active collaboration between dialysis facilities and transplant centers will be needed to establish a firm foundation for achieving meaningful outcomes for patients who are interested in transplantation as a modality for treating ESRD.
FIGURE 1 | Levels of intervention within the RaDIANT Community Study
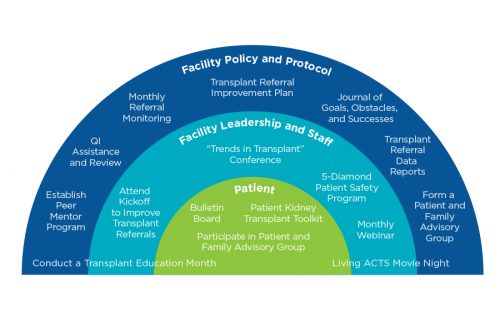
FIGURE 2 | Adjusted mean proportion of dialysis facility referrals for RaDIANT Community Study intervention group versus control group among the black and white patient population within dialysis facilities at baseline (2013) and after the intervention (2014).

COLLABORATION OPPORTUNITIES: NEXT STEPS
The FMCNA Medical Office is actively engaged with the leadership of the American Society of Transplant Surgeons (ASTS) to determine how to increase Fresenius Kidney Care patient access to transplantation through strategies such as:
- Identifying transplant referral trends and opportunities for improvement at all Fresenius Kidney Care centers
- Improving communication between Fresenius Kidney Care centers and transplant centers to track patient progress through the transplant evaluation process and the patient’s status on the transplant list
- Collaborating with transplant centers on identifying transplant candidates, providing education, and improving arteriovenous fistula (AVF) rates, or on an alternative safe, planned return to dialysis if a transplant fails
PROPOSED CHANGE
Unfortunately, not all ESRD patients are candidates for transplant, but all ESRD patients benefit from a well-functioning permanent vascular access. Rather than focusing on the dialysis clinic’s absolute transplant referral rate as a quality metric, it may be more advantageous to partner with transplant center personnel—inviting them into Fresenius Kidney Care dialysis centers to perform chart reviews, offer chairside transplant education to patients, and initiate transplant referrals for appropriate candidates. The presence of transplant center personnel in the dialysis facility can serve other purposes, including increasing vascular access placement by performing point-of-care vein mapping at the dialysis facility and providing education on the benefits of a well- functioning fistula.
FMCNA is collaborating with the ASTS to ensure AVF creation training is a core competency for ASTS-certified transplant surgery training programs. FMCNA is also working closely with the ASTS and Fresenius Vascular Care to provide post-graduate training for transplant surgeons who could supplement their core specialties supporting better vascular access care.
Meet the Author
BENJAMIN HIPPEN, MD, FASN, FAST
Medical Director, Fresenius Kidney Care
Partner, Metrolina Nephrology Associates
Clinical Professor, Dept. of Medicine, UNC-Chapel Hill School of Medicine
Dr. Hippen is a general and transplant nephrologist with Metrolina Nephrology Associates, P.A. He is also the associate medical director of the kidney and kidney-pancreas transplant program at the Carolinas Medical Center and serves as medical director of an Fresenius Kidney Care in-center hemodialysis and home therapies facility in Charlotte, North Carolina.
References
- Department of Health and Human Services. Medicare program: conditions for coverage for end- stage renal disease facilities—third party payment. Federal Register. Part 494. 2016 December 14;81(240). https://www.gpo.gov/fdsys/pkg/FR-2016-12-14/pdf/2016-30016.pdf.
- Patzer RE et al. The RaDIANT Community Study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrology. 2014;15:171. http://bmcnephrol.biomedcentral.com/articles/10.1186/1471- 2369-15-171#Fig2.
- Patzer RE et al. Variation in dialysis facility referral for kidney transplantation among patients with end-stage renal disease in Georgia. JAMA. 2015 August 11;314(6):582-594.
- Patzer RE et al. A randomized trial to reduce disparities in referral for transplant evaluation. JASN. Published online before print October 13, 2016. http://jasn.asnjournals. org/content/early/2016/10/12/ASN.2016030320.full. See especially Supplemental Appendix 3 for further detail on the several interventions in the RaDIANT study, available at http://jasn.asnjournals.org/content/early/2016/10/12/ASN.2016030320/suppl/ DCSupplemental.
- Department of Health and Human Services. Kidney allocation system. https://optn. transplant.hrsa.gov/learn/professional-education/kidney-allocation-system/. Accessed March 26, 2017.


