Leading Innovation Through Value Based Care
As the leader in value based care (VBC) for patients with end stage renal disease (ESRD), Fresenius Medical Care North America (FMCNA) is in an ideal position to drive healthcare innovation. FMCNA has already had success in reducing cost while advancing care coordination to keep patients healthy, compliant with dialysis, and ambulatory. Because these programs are designed for renal patients with complex conditions, FMCNA's infrastructure and technology are particularly well suited to broader patient populations with chronic conditions. FMCNA is also anticipating the next generation of VBC programs that will offer additional services while reducing costs.
As VBC has evolved and matured over the past decade, one thing has become certain: It is here to stay. FMCNA's outlook on the transition from volume- to value based healthcare includes these key points:
- VBC has grown tremendously across the entire U.S. healthcare continuum.
- FMCNA is the leader in VBC for patients with ESRD.
- Condition-specific interventions are successful in delivering VBC.
- FMCNA is positioned to innovate as VBC evolves.
VBC Has Grown Tremendously Across the Entire US Healthcare Continuum
Programs such as Medicare and commercial accountable care organizations (ACO), bundled payments, private, and federal insurance exchanges, Medicaid program expansion, Medicare Access and the CHIP Reauthorization Act of 2015 (MACRA), and vertical delivery integrations are a few of the healthcare delivery innovations that have expanded greatly during the past several years. These programs are designed to achieve improved health quality outcomes and reduce wasteful healthcare (therefore creating value). Fresenius Health Partners (FHP) is the FMCNA population health entity convening those innovations for the company's renal disease patients.
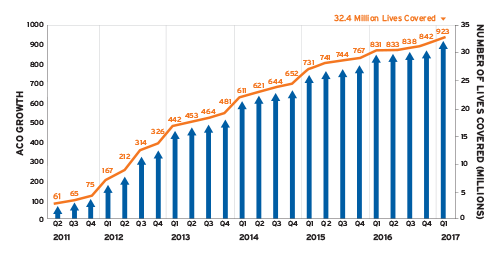
Through FHP, FMCNA has been investing in VBC programs for over a decade, but it is only in the last few years that the healthcare market norm has moved toward these programs and driven significant growth within FHP (Figure 1).1
FIGURE 1 | Growth of payment reform programs shows a year-over-year increase in the number of public and private accountable care programs
FMCNA Is the Leader in VBC for Patients with ESRD
Policy analysts have been reviewing performance results of accountable care programs to determine why certain programs succeed where others fail. This will be an ongoing process across the industry, but FMCNA perceives there is a significant ability to positively impact its patients by being an early adopter before the policy analysts reach a conclusion. Overall, high-functioning markets have had better success than fragmented markets, and there are indications that disease-specific population health management may achieve greater results.
As a result, FHP is focusing resources on significant opportunities in these two spaces: vertically integrated healthcare delivery and disease-specific population health management. FHP's growth in the past few years has had three drivers: the launch of an ESRD Chronic Condition Special Needs Plan (C-SNP) Medicare Advantage program; participation in the Center for Medicare and Medicaid Innovation's (CMMI) Comprehensive ESRD Care (CEC) program; and partnerships with several commercial payers to manage FMCNA ESRD populations through vertical integration of care and emphasis on care coordination for patients with ESRD.
FMCNA, as well as other CEC participants, achieved significant reductions in the total cost of care for patients across these programs as demonstrated in Figure 2.
FIGURE 2 | CEC program participant shared savings vs benchmark (per member per year)
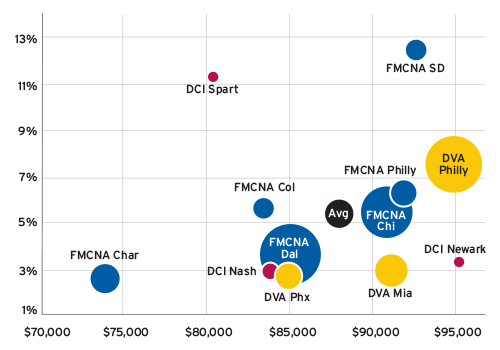
Source: Data used to create figure is available at https://innovation.cms.gov/Files/x/cec-fncl-py1.pdf
The number of FHP's patients participating in the CEC program increased from 8,000 in 2016 to 26,000 in 2017—and exceeds approximately 40,000 patients in 2018. FHP's attributed patients with ESRD exceeds all other CEC participants and is evidence that FMCNA is committed to the CEC program and VBC initiatives.
To achieve success, FHP has focused resources on coordinating care for the patient with ESRD beyond the four walls of the dialysis center. Care coordination is a combination of close communication with nurse case managers, social workers, pharmacists, behavioral health specialists, hospitalists, and multiple provider specialists. Sophisticated data analysis and predictive modeling are also important elements, especially when managing an ESRD population where half of the patients will be hospitalized each year. This focus on care coordination has created vertically integrated care in several FMCNA markets and has shifted the focus of the patient from one that was renal-centric to one that is patient-centric. Care coordination focuses on keeping the patient healthy, compliant with dialysis, and ambulatory.
Condition-Specific Interventions Are Successful in Delivering VBC
The dialysis patient's health situation is typically complex, arguably the most complex chronic condition because it requires so much of a patient's time. Ten or more hours per week are spent in hemodialysis treatment. This "contact time" affords FHP and its partners the opportunity to positively influence outcomes for patients with ESRD by engaging patients through education and coaching them on healthier lifestyles. FHP programs are uniquely designed for renal patients, whether it be regular transportation to recurring visits, reducing the risk of bloodstream infections, vascular access flow surveillance, or adherence to dialysis. Because of this, FHP can focus interventions on preventing or minimizing those disease exacerbations that lead to frequent hospitalization. Since FMCNA is vertically integrated, the company can accomplish more efficient, just-in-time, healthcare delivery that fragmented systems cannot provide as effectively.
One example of disease-specific integrated care is treatment surveillance and adherence. FHP has developed programs that encourage providers to engage patients at their greatest time of need—during transitions to and from the hospital. FHP has invested in technology that allows its Care Navigation Unit (CNU) to be notified when a patient is not at a scheduled dialysis appointment and when the patient registers at the hospital emergency department. Upon notification, the CNU nurses reach out to the patient and/or the hospital to assist with any of the patient's acute needs.
Success with specific diseases is not limited to ESRD. Many chronic conditions, such as congestive heart failure, and diabetes, are poised to see significant benefit in VBC. While designed for renal patients, FHP's infrastructure and technology are well suited to serve other patient populations.
VBC affords flexibility to create programs to improve outcomes that would not be possible under traditional reimbursement mechanisms. One example includes screening patients for diabetic retinopathy. FHP acquired technology and trained staff to obtain images of diabetic patients' retinas. These images are reviewed by an ophthalmologist to screen for and detect changes in a patient's retina caused by diabetes. Early referral and treatment can delay or prevent vision loss. A value based program such as the CEC Model allows FHP a funding mechanism for the technology and staff time to screen for diabetic retinopathy.
FMCNA Is Positioned to Innovate as VBC Evolves
As FHP looks to the future, it will build upon its established foundation. Incentivizing providers and partner delivery systems is both a challenge and an opportunity. Providers with a significant portion of their patients insured under traditional Medicare are subject to the Quality Payment Program (QPP). By design, the QPP creates financial incentives for participation in Advanced Alternative Payment Models (AAPM). The alternative is exposure to the Merit-Based Incentive Payment System (MIPS). Providers that participate in AAPMs and achieve Qualifying Participant status benefit as they are excluded from MIPS and collect a 5 percent bonus on their fee-for-service billing to Medicare. The financial consequences of not participating in the QPP become greater each successive year of nonparticipation.
Providers that manage chronic diseases, specifically nephrologists, cardiologists, and PCPs, no longer can embrace status quo and need to participate in an APM to maintain their current revenues from federal programs. FHP anticipates that the AAPMs will evolve over time but are unlikely to be rescinded. Nephrology is one of the few areas with a specialty-specific AAPM, creating a strong incentive for nephrologists to participate in FHP's CEC programs. In 2017, over 800 nephrology providers met the criteria to be a qualified participant in an AAPM through the FHP CECs.
Medicare is expected to seek further payment reform with more progressive VBC programs offered through CMMI. Over time, CMMI will focus on programs that generate the most value, and FMCNA projects this will include programs that target disease-specific populations like ESRD. FMCNA supports innovation and knows that larger programs covering the broadest percentage of patients will allow providers to modify their practice in a meaningful way to meet the program goals. The next generation of renal programs may have an even greater impact on patient outcomes. Programs will be designed to address seamless access to care and efficient care transitions, as well as protect patient choice and minimize impact on patient convenience while allowing providers the best levers possible to improve outcomes and lower costs.
More than just care coordination, these next-generation programs will allow providers to offer additional services to enhance quality while reducing costs. Dental care, which reduces the risk of infection from dental disease, may improve patient qualification for transplant. In addition, access to over-the-counter drug benefits will allow patients to obtain many of the medical items often needed by the dialysis population. Vision benefits may be included to assist the large number of diabetics within this population.
FHP population health programs are well suited to reach the broader ESRD population of FMCNA, but are also designed to push toward the future, embracing the next generation of VBC. The company will continually evolve its strategies and care management programs to maintain its position as the leading innovator in ESRD value based care.
Change is everywhere in healthcare. Healthcare reform is no longer just getting started, and value based care through payment innovation is the new norm. FHP is perfectly positioned to be on the forefront of population health reform to the benefits of Fresenius Kidney Care patients, partners, and employees.
Meet Our Experts
Andrew Aronson, MD, FACEP
Vice President, Senior Medical Director, Fresenius Health Partners
Andy Aronson oversees the clinical aspects of the Medicare Advantage Chronic Special Needs Plans, ESRD Seamless Care Organizations, and the commercial ESRD programs. He is a Board-Certified Emergency Physician, a fellow of the American College of Emergency Physicians, and an editor of the Journal of Population Health Management. He completed medical school at Drexel University College of Medicine and emergency medicine residency at Brigham & Women's Hospital and Massachusetts General Hospital.
William McKinney
President, Integrated Care Group, Fresenius Medical Care
William McKinney is president of Integrated Care Group, which includes Fresenius Health Partners and FreseniusRx. He launched FMCNA's health plan as the president of Fresenius Health Partners in 2014 and 2015. McKinney holds bachelor's degrees in computer engineering and mathematics from Southern Methodist University in Dallas.
References
- Muhlestein D, Saunders R, McClellan M. Growth of ACOs and alternative payment models in 2017. Health Affairs (blog), June 28, 2017. https://www.healthaffairs.org/do/10.1377/hblog20170628.060719/full/.
- Centers for Medicare & Medicaid Services (CMS). Comprehensive ESRD Care Model. Last updated April 16, 2018. https://innovation.cms.gov/initiatives/comprehensive-esrd-care/.
- CMS Innovation Center. Comprehensive ESRD Care Model (CEC Model) fact sheet. Accessed March 30, 2018. https://innovation.cms.gov/Files/fact-sheet/cec-fs.pdf.
- Ibid.
- Comprehensive ESRD Care Model. https://innovation.cms.gov/initiatives/comprehensive-esrd-care/.



