Using AI to Predict Patient Outcomes | FMCNA
An interview with Len Usvyat, Vice President of Integrated Care Analytics at Fresenius Medical Care North America, about the increasing importance of artificial intelligence to deliver new insights that improve outcomes for our patients.
Q: How would you describe your role at Fresenius Medical Care?
LU: My team’s role is to bring innovative thinking about data to every corner of this organization, both on the clinical and operational sides. Our mission is to look for signals in the data and translate them into actionable insights that can be used by clinicians, nurses and doctors.
I began my career in accounting, and I learned a lot about numbers. However, I felt like there was no human touch to that data. After joining the Renal Research Institute in the early 2000s, I fell in love with the idea that behind every number, there is a real patient with his or her own feelings and emotions. A life we can positively impact.
Q: How important is machine learning and artificial intelligence been to improving care for our patients?
LU: Our senior leadership believes the use of data and artificial intelligence (AI) is vital to improving how we care for our patients. As we advance our expertise in this field, we are learning how to use data and the resulting interventions more intelligently. Hundreds of large companies and start up organizations are using artificial intelligence to improve health care delivery and we must not fall behind in that evolution. Our team is working hard to build a strong foundation for machine learning and predictive analytics.
Q: Several abstracts at ASN Kidney Week this year show how machine learning can predict outcomes for our dialysis patients. One of your team’s efforts is to predict, intervene and prevent hospitalizations. How does this model work?
LU: Hospitalization is a huge issue for dialysis patients. On average they are hospitalized almost twice a year. Hospitalizations result in missed treatments, decreased quality of life and higher costs to the whole health care system.
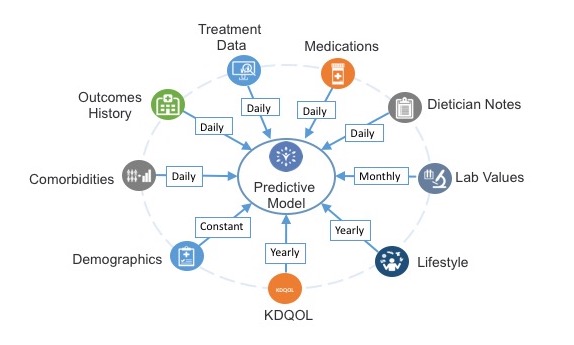
We have built a model that aims to predict when a patient may go to a hospital within the next week. Our team built a code that extracts nearly 1,600 variables every night including nursing notes about the treatment itself. We have programmed the computer to automatically process those variables and predict whether a patient will go to the hospital in the next week. We are now in the third phase of this pilot.
While the model provides an accurate prediction, we are now looking at whether the associated interventions can reduce the number of hospitalizations. So, while the first steps have gone very well, we are now putting that model to work in our clinics. By doing so, we are helping our clinicians get used to the idea that there may be signals in all that data that no human can possibly process or see.
Q: Another abstract presented this year is about using machine learning to predict infection for patients using peritoneal dialysis. How can that help us increase the number of patients on home dialysis?
LU: One of the biggest issues for patients who dialyze at home is the potential for infection. It’s not just about getting people to switch to home dialysis, it’s about getting them to stay on that modality and be successful.
Peritonitis is one of the top factors for why patients are unable to continue peritoneal dialysis at home. Can we use the wealth of data at our disposal to better predict when patients will have an infection? We are starting to see some early positive results on a predictive model that looks out about a month in advance. The next phase will be seeing whether we can use those insights to actually prevent peritonitis episodes. Possible interventions may include proactively visiting patients at the highest risk for peritonitis in the next month or increased testing to identify and treat infections early.
Q: This must be an exciting time to be a data expert in health care?
LU: It’s an unquestionably exciting time to be working with data and machine learning. But the challenge now is to introduce these novel concepts to clinicians, be it medical doctors, nurses or PCTs who are not as familiar with these concepts. We need to break through the traditional way health care has always been delivered and demonstrate that there may be new ways to do things. These innovative methods only aim to supplement the work already done by our clinicians.
We are currently seeing incremental changes that introduce predictive analytics to improve care. Up until a few years ago, every physician had to actively calculate dosing adjustments of a drug to treat anemia. But with some computerized algorithms developed by the Renal Research Institute and Fresenius’ data analytics team, physicians now can simply oversee automated dosing adjustments, saving them time and allowing them to focus on other patient concerns. This is a classic example of how an incremental change can make a big impact.
It will take time, but in the next twenty years I believe we will be relying much more on these tools to help support routine clinical decisions.
About Len Usvyat, Vice President of Integrated Care Analytics
Len is responsible for supporting analytical efforts across Fresenius Medical Care North America (FMCNA) including predictive modeling, outcomes analysis, and research. Len has over 15 years of experience in data management, analytics, research, and epidemiology. He previously worked with Renal Research Institute, an FMCNA subsidiary, on a variety of projects related to patient outcomes and quality reporting. Len has published over 40 manuscripts in peer reviewed journals. He holds a master’s degree from the University of Pennsylvania and a Ph.D. from the University of Maastricht in the Netherlands.
RESOURCES:
Listening Through Numbers by Len Usyvat


